Health & Wellness Blog
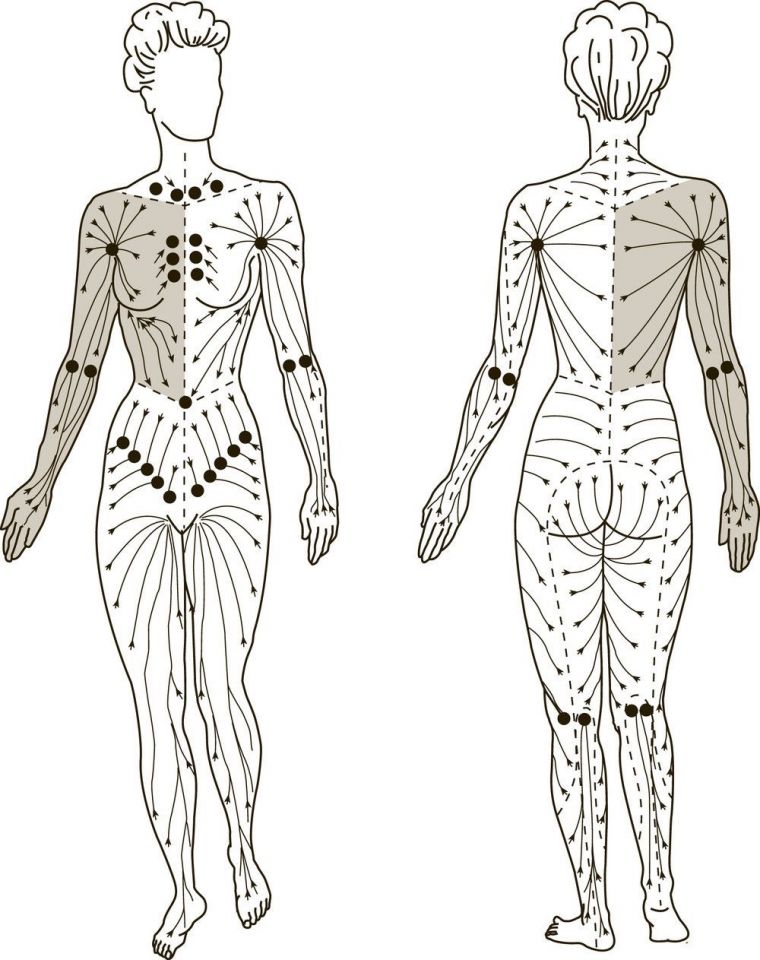
Manual Lymphatic Drainage: A Gently Way to Support your Health
Written by Joelle Renwick, May 2025
Understanding Autism Spectrum Disorder in Women
Written by Joelle Renwick, December 21, 2024
Stress and its Effects on the Brain and Body:
A Deep Dive into the Biological and Physiological Mechanisms of stress
Written by Joelle Renwick, October 16, 2023
.png)